In the last ten years, there has been an honest and brave openness in discussing mental health. A discussion often promoted by well-known and respected figures from the sport and art industries who have been sharing their own experiences about living with mental illness and trying to overcome it (Michael Phelps, Dewayne “the rock” Johnson, Ian Thorpe, Ricky Hutton, Serena Williams, Emma Stone, JK Rowling, Halle Berry, Prince Harry… just to name a few who have publicly spoken about their mental challenges)
According to Mind UK, 1 in 4 people in the UK will experience a mental health problem each year, and each of us knows someone who is or has been suffering from mental illness.
Raising awareness of how prevalent the problem is has helped to decrease the stigma once attached to mental disorders, and it has increased the research in understanding the causes and finding possible solutions.
Many factors, such as biology (genetics and brain chemistry) and life experiences (trauma, abuse) contribute to mental health problems. Therefore a successful approach to recovery must include a variety of interventions such as cognitive behavioural therapies, resilience-building activities, psychotherapy, yoga, relaxation techniques, exercise and on a biochemical level, science has shown how nutrition, can play a significant role, in improving and supporting the healing.
Indeed, there is no doubt about the connection between the food we eat and the way we feel, in the short and long term.

Blood sugar balance and mental health
Anxiety, mood swings, depression and dementia, are negatively affected by imbalanced blood sugar levels and regulating the amount of sugar in circulation in our bloodstream is the first essential step we can take to improve our mental wellbeing.
However, this is not so easy because when we feel stressed or low, the type of foods which give us an immediate lift in energy or comfort are the foods rich in simple sugars and fat. These foods can activate the reward system in the brain via the opioid, dopamine, and endocannabinoid systems, the systems responsible for influencing instinct, moods and pleasure. So, when you eat that pain au chocolate in the morning, you’re affecting these systems, in a way that makes you feel good in the short term and reinforce a behavioural loop which makes you think that to feel better you need to eat that type of food!
Unfortunately, in the long term, this will not be helpful; on the contrary, it can become one of the factors involved in the development of mental imbalances. A chronically high amount of sugars in the bloodstream will lead to elevated secretion of insulin, a pro-inflammatory hormone, and eventually, the insulin will no longer have the desired effect of disposing of sugar into our cells. This condition, called insulin resistance, if not addressed, will lead to diabetes type2. The inability of delivering glucose in the cell, can affect the supply of energy and make us feel tired, depleted, hungry, low, irritable and craving for more sugar!
Our brain health is also directly influenced by our blood sugar balance. The brains primary function of processing and transmitting information through electrical signals is costly in terms of energy use and relies on a constant supply of oxygen and glucose (it can also utilise ketones very effectively … this is the topic for another blog). The link between insulin resistance and dementia is very well established, and Alzheimer is often referred to as diabetes type 3.
Blood sugar balance and brain health: start here
The way to balance blood sugar levels is to adopt a low glycaemic load (low GL) eating style, and you can start by simply applying the following guidelines:
- Eat regularly – you might need to start with three main meals per day and two regular snacks in-between. The goal is to progress to 3 or 2 main meals per day without food in between; this will take a while, especially if your blood sugar is very imbalanced at the moment. I have clients who thrive with two meals only per day and clients who absolutely need 3, remember we are all unique, and one rule does not fit all. Your meal requirements also depend on your exercise routine. One thing that is absolutely a no-go is grazing from meal to meal!
- Avoid foods which are highly processed and refined – anything made with white refined flours and grains ( white rice, bread, pasta, biscuits, crackers, scones, certain types of breakfast cereals); anything that is high in added sugar ( chocolate bars, candies, cereal bars, fruit yoghurt, soft drinks).
- If you juice, avoid fruit juices but instead opt for juices made prevalently with green vegetables; keep your dry fruit to a minimum (raisins, dates, dry cranberries, dry fruit, they contains a very high amount of glucose and fructose)
- Have balanced meals with proteins, healthy fats (from avocados, olive oil, nuts and seed, coconut yoghurt, oily fish ) and slow-releasing carbs ( these are the carbs you get from non-starchy vegs)
- Make the first meal of the day rich in proteins and healthy fats rather than focused on carbs; this is a widespread mistake and leads to more carbs cravings later in the day.
If you want to read more in detail about blood sugar balancing, click here to read my blog on low glycemic eating style.

What your brain needs for optimal function
The eating style:
Adopt a low glycemic load eating style to regulate and maintain blood sugar levels; in more advanced phases, you might consider progressing to a healthy ketogenic eating style. I will be writing on this in future blogs. But start with mastering a low glycemic load style first, the transition to keto will be much easier.
Vitamins and minerals: the essentials
Multivitamins, B complex, vitamin C, magnesium, vitamin D
Several studies show that taking multivitamins regularly can help reduce stress, anxiety, aggression, low moods, autism and ADHD.
A study involving 129 healthy young adults taking a multivitamin formula for 12 months reported significantly improved moods feeling more agreeable, more composed and reported better mental health.
B vitamins delay brain atrophy and have been studied for their positive effect in increasing cognitive function and resilience to stress.
Vitamin C is very supportive in reducing mood disturbance, fatigue and higher amount of plasma vitamin C are associated with improved cognitive functions.
The first evidence for the use of magnesium in patients suffering from depression was published almost 100 years ago, and modern research has confirmed the efficacy of magnesium supplementation in supporting those recovering from depression. Magnesium is also beneficial during periods of high stress as it helps the body and mind to relax.

Catch the rays and if you can’t, supplement!
The role of Vitamin D is well known in relation to bone health and immunity; however, it also performs a hugely important role in mental health. Vitamin D, which behaves more like a hormone than a vitamin, reduces toxicity and inflammation in the brain and is one of the vital nutrients that must be considered in the prevention of dementia. If you are living in the UK, there is no doubt that you are not getting the optimal level of vitamin D. I always recommend my clients to get tested at least once a year to establish the baseline level and start supplementation accordingly. Getting tested for vitamin D can be done by ordering a prick finger test online. I use a lab called Thriva, it’s cheap and easy and a critical assessment to have done.

Get fat smart! Focus on Omega-3 and phospholipids
Two thirds of brain dry weight is fat of which ¼ is an Omega-3 fat called DHA. DHA intake, found in oily fish (salmon, anchovies, mackerel, sardines) and algae extract ( in a supplement form suitable for vegetarian and vegan ), is positively correlated with brain volume. It is an essential component of neurons membranes, stimulates neurogenesis (the growth of new neurons) and is a brain antioxidant.
Research shows that daily Omega-3 supplementation of DHA and EPA is supportive in reducing anxiety, depression, improves antisocial behaviours, psychosis and better neurocognitive performance under stress.
Phospholipids are perhaps the less know type of fats and don’t often get the attention they deserve, however, these type of fats are extremely important for healthy nerve cell membranes which play a significant role in neurotransmission ( the communication between neurons). Phosphatidylserine, in particular, can slow, halt and reverse biochemical changes and deterioration in nerve cells. In the diet, we get it from animal sources ( chicken and beef liver are particularly rich in it ), fish, egg yolks, soybeans, sunflower seeds.

Eat a rainbow for a load of phytonutrients: your powerful plant pharmacy
Phytonutrients are naturally occurring plant chemicals which have a beneficial effect on our health. Plants that have been grown organically have a higher content of phytochemicals which they produce as a form of defence against attacks from the environment (insects, heat, infections etc.)
Research shows that higher consumption of vegetables rather than fruit is associated with decreased risk of dementia and cognitive decline. We need seven portions per day at least, but for optimal health, experts recommend as much as 10 per day, and I agree with that. However, for most of us, a more realistic approach is 7 of which 5 vegs and 2 fruit portions. A vegetable portion is considered 80g, and one portion of fruit, 150g.
When it comes to brain health and content of phytochemicals the champions from the plant kingdoms are berries, raw cacao, green leafy vegetables, herbs and spices and green tea.
The different colours in plants represent different phytochemicals, that is why eating a rainbow is THE thing to do!
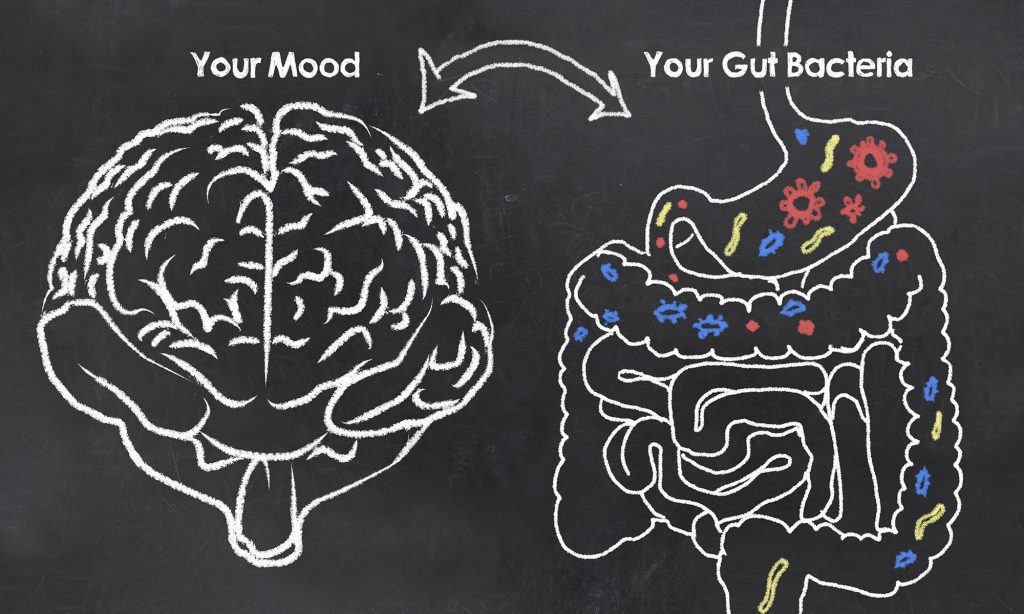
The gut-brain link
Your brain health is strictly related to the health of your gut, and when we think brain, we should automatically think of the microbiome. The microbiome is the collection of trillions of micro-organisms living in our gut. It has direct communication to the brain via a bidirectional highway. The brain and the gut are constantly in contact with each other in many different ways, and it is not a surprise, that the number of messages coming from the microbiome to the brain is 400 times as much than the other way round! This means that by improving the quality of our microbiome, we can influence the messages and improve brain health!
Foods which play a significant role in gut health are the prebiotics and probiotics foods. Prebiotics foods are rich in a type of fibres that the beneficial bacteria love to feed on, asparagus, green bananas, aubergine, endive, garlic, Jerusalem artichokes, leeks, legumes, onions, peas and radicchio.
Probiotics foods contain good bacteria and help colonisation of the digestive tract, yoghurt, kefir, sour cream, cheese, fomented vegetables, kimchi, kombucha, miso, natto, tempeh.
I recommend that you include some of these foods daily into your diet. Start with a small amount of prebiotics foods and slowly build up as they might cause some bloating and flatulence until your system gets used to them.

Give yourself permission to take care of … yourself J
Depending on the specific mental challenges and goals, there are other nutritional interventions that can be added to the above. As I said before, one size does not fit all, especially when it comes to nutrition; I always recommend seeing a qualified and registered nutritional therapist to discuss your particular individual needs.
Finally, in my practice, I meet many people, and in particular women, that find it difficult to prioritise their needs because they perceive focusing on their physical and mental wellbeing as being selfish and indulgent. This is far from the truth! In fact, the truth is that, if we don’t honour our body and mind with nourishment, exercise, mindfulness and relaxation, this will, not only reflect negatively on our mental health, but also in the wellbeing of the people around us.
So, if you can’t practice self-care just for yourself, practice self-care for the people you love.
Wishing you the best of health and vitality,

References:
Crawford M, A, Bazinet R, P, Sinclair A, J: Fat Intake and CNS Functioning: Ageing and Disease. Ann Nutr Metab 2009; 55:202-228. doi: 10.1159/000229003.
Diehl, T., Mullins, R., & Kapogiannis, D. (2016). Insulin resistance in Alzheimer’s disease. Translational research : the journal of laboratory and clinical medicine,183, 26-40.
George AE and Karen LE (2006) Rapid recovery from major depression using magnesium treatment,
Glade MJ and Smith K (2014) Phosphatidylserine and the human brain. Nutrition. 2015 Jun;31(6):781-6. doi: 10.1016/j.nut.2014.10.014.
Grosso, G., Pajak, A., Marventano, S., Castellano, S., Galvano, F., Bucolo, C., Drago, F., & Caraci, F. (2014). Role of omega-3 fatty acids in the treatment of depressive disorders: a comprehensive meta-analysis of randomized clinical trials. PloS one, 9(5), e96905.
Haan, MN et al (2007) Homocysteine, B vitamins and the incidence of dementia and cognitive impairment: results from the Sacramento area Latino study on aging. American Journal of Clinical Nutrition,85:511-517.
Hibbeln JR et al. (2006) Omega-3 fatty acid deficiencies in neurodevelopment, aggression and autonomic dysregulation: Opportunities for intervention. International Review of Psychiatry, volume 18, 2.
Hoffer, L.J. (2008) Vitamin therapy in schizophrenia. Israel Journal of Psychiatry and Related Sciences, 45(1), p.3.
Kennedy, D.O., Veasey, R.C., Watson, A.W., Dodd, F.L., Jones, E.K., Tiplady, B. and Haskell, C.F. (2011), Vitamins and psychological functioning: a mobile phone assessment of the effects of a B vitamin complex, vitamin C and minerals on cognitive performance and subjective mood and energy. Hum. Psychopharmacol Clin Exp, 26: 338-347.
Kieboomet et al. (2017) Serum magnesium is associated with the risk of dementia. Neurology 89 (16): 1716-1722.
Li W et al. (2014). Elevation of brain magnesium prevents synaptic loss and reverses cognitive deficits in Alzheimer’s disease mouse model. Molecular brain,7, 65. doi:10.1186/s13041-014.
McDonald, T., & Cervenka, M. C. (2018). The Expanding Role of Ketogenic Diets in Adult Neurological Disorders.Brain sciences,8(8), 148. doi:10.3390/brainsci8080148.
McNamara, R. K., & Strawn, J. R. (2013). Role of Long-Chain Omega-3 Fatty Acids in Psychiatric Practice. PharmaNutrition, 1(2), 41–49.
Mullins, R. J., Diehl, T. C., Chia, C. W., & Kapogiannis, D. (2017). Insulin Resistance as a Link between Amyloid-Beta and Tau Pathologies in Alzheimer’s Disease.Frontiers in aging neuroscience,9, 118. doi:10.3389/fnagi.2017.00118.
Pinto A e al. (2018) Anti-Oxidant and Anti-Inflammatory Activity of Ketogenic Diet: New Perspectives for Neuroprotection in Alzheimer’s Disease. Antioxidants 7(63):doi:10.3390/antiox7050063.
Raine, A., Portnoy, J., Liu, J., Mahoomed, T., & Hibbeln, J. R. (2015). Reduction in behavior problems with omega-3 supplementation in children aged 8-16 years: a randomized, double-blind, placebo-controlled, stratified, parallel-group trial. Journal of child psychology and psychiatry, and allied disciplines, 56(5), 509–520.
Rutklidge JJ and Kaplan BJ (2013) Broad-spectrum micronutrient formulas for the treatment of psychiatric symptoms: a systematic review. Expert Rev Neurother. 2013 Jan;13(1):49-73. doi: 10.1586/ern.12.143.
Serefko A et al. (2013) Magnesium in depression. Pharmacol Rep. 2013;65(3):547-54.
Smith AD and Refsum H (2016) Homocysteine, B Vitamins and Cognitive impairment. Annual Reviews in Nutrition, 36:211-239.
Steen et al. (2005) Impaired insulin and insulin-like growth factor expression and signalling mechanisms in Alzheimer’s disease –is this type 3 diabetes? Journal of Alzheimer’s Disease,7, 1:63-80.
Stephen C. Cunnane, Michael A. Crawford ( 2014) Energetic and nutritional constraints on infant brain development: Implications for brain expansion during human evolution, Journal of Human Evolution,
Volume 77, 88-98, ISSN 0047-2484.
Zhang M at al. (2011) Vitamin C provision improves mood in acutely hospitalized patients, Nutrition, Volume 27 (5), 530-533, ISSN 0899-9007.




Hi Monica
Yesterday I was told that it is a good idea to have a NHS dexa scan to test for osteoporosis and that you can just ask for one. Is that true? Secondly do you think that every woman who has gone through the menopause should take HRT for life? Really not sure and do not like the idea of taking a hormone daily but perhaps it is better to keep oestrogen levels up. Am interested to know what you think?
Hope all is well with you
Are you now in London rather than Windsor?
Take care and many thanks
Lorraine